Download ECGs, Illustrations, and other Resources for your classes.
ALL OUR CONTENT IS FREE OF CHARGE AND FREE OF COPYRIGHT IF USED IN A CLASSROOM SETTING
ECG Challenge from
Limmer Creative & ECG Guru

Great practice strips for your students. Easy to use app for your mobile device
GET THE APPECG & ILLUSTRATIONS ARCHIVES SEARCH (SCROLLABLE LIST)
Dawn’s Classes
ECG Guru Ads - Products and Services of Interest to our Members
If you would like to place ads for products or services of interest to our readers, please contact us at [email protected]
ECG HISTORY: ECG was first put into clinical use in the early 1900s. In 1909, it helped diagnose an arrhythmia. A year later, indications of a heart attack were noted.
-
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.
Recent blog posts
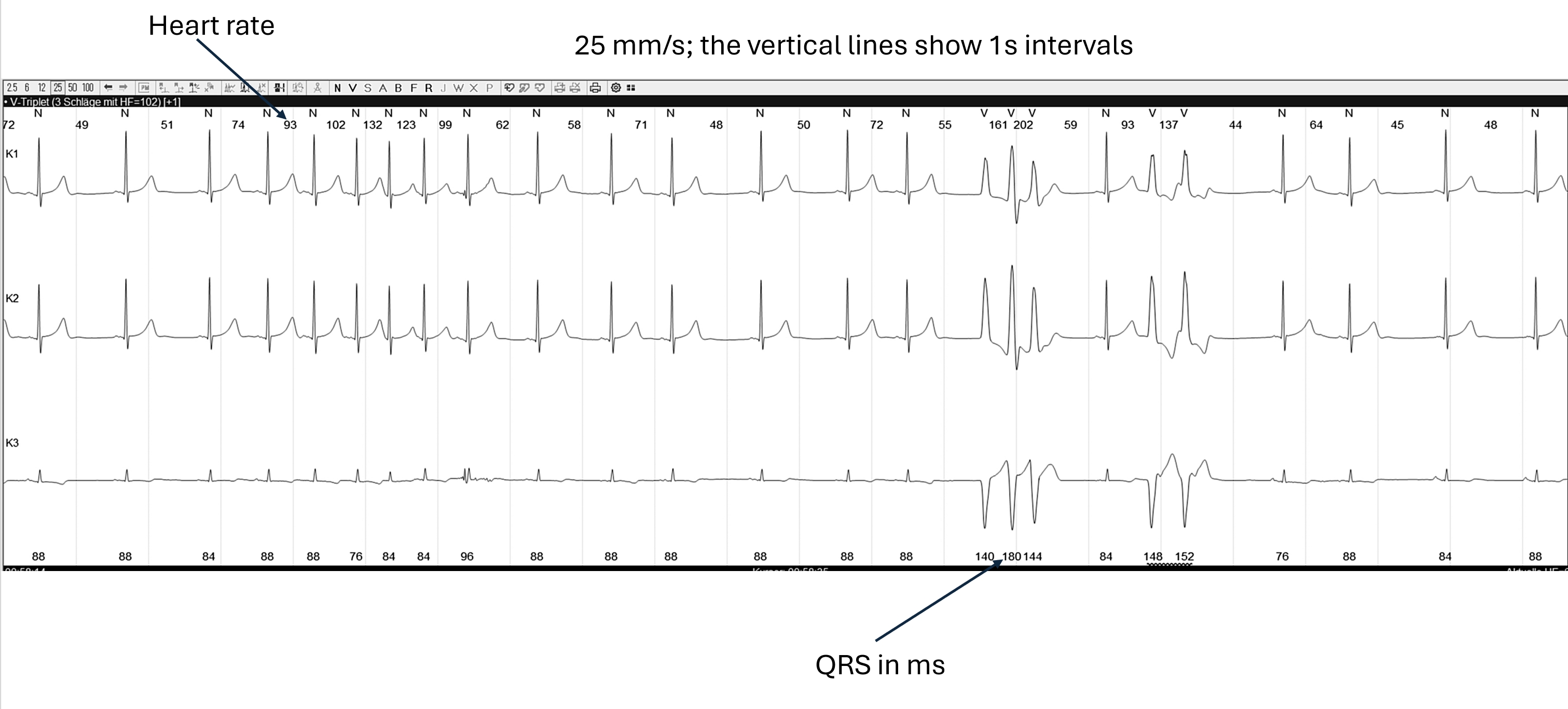
- An Interesting Holter Strip
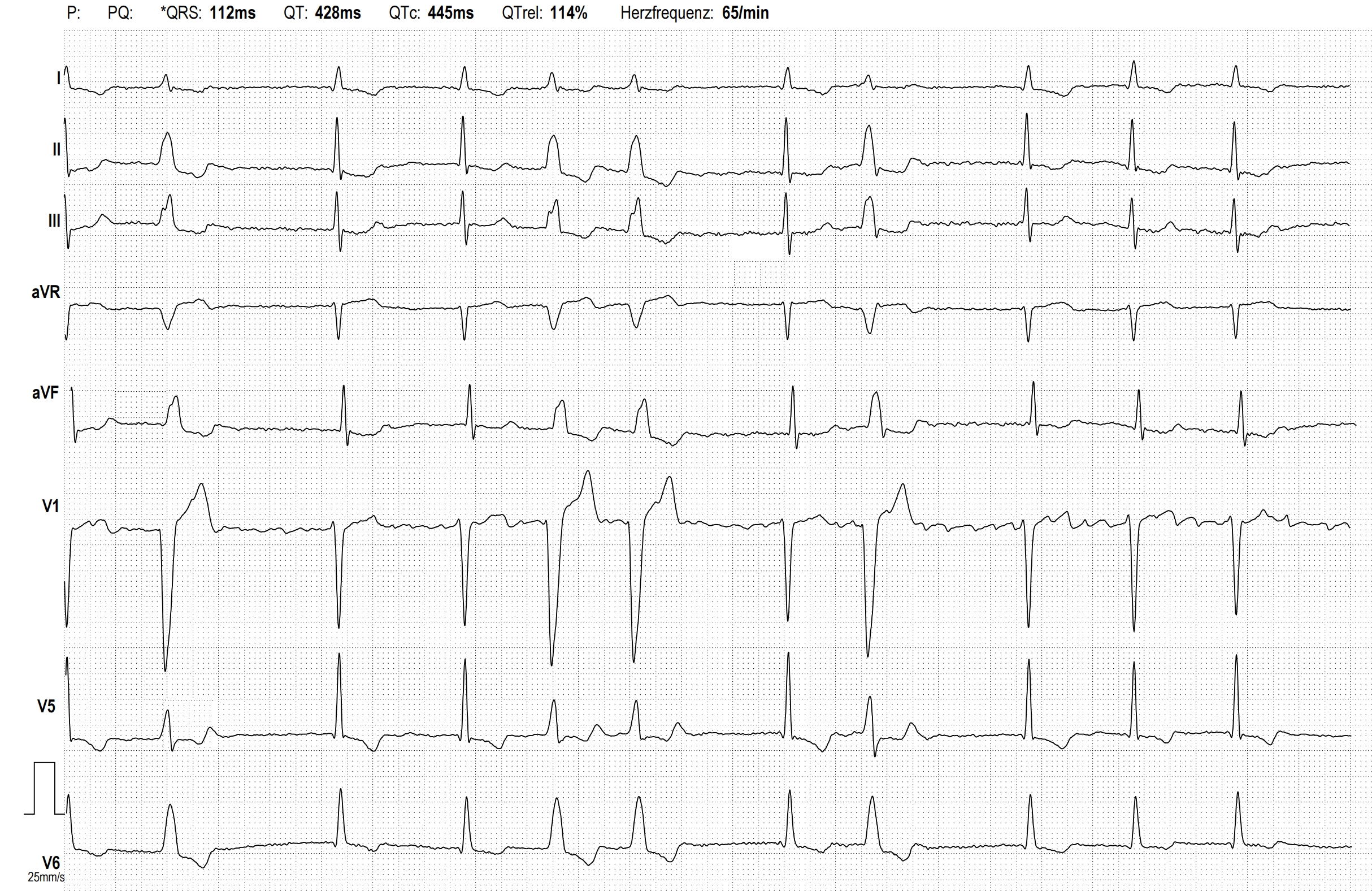
- Atrial Fibrillation With Rate-related Left Bundle Branch Block
- New Book From Dr. Jerry Jones
- VENTRICULAR TACHYCARDIA WITH SUCCESSFUL ATP
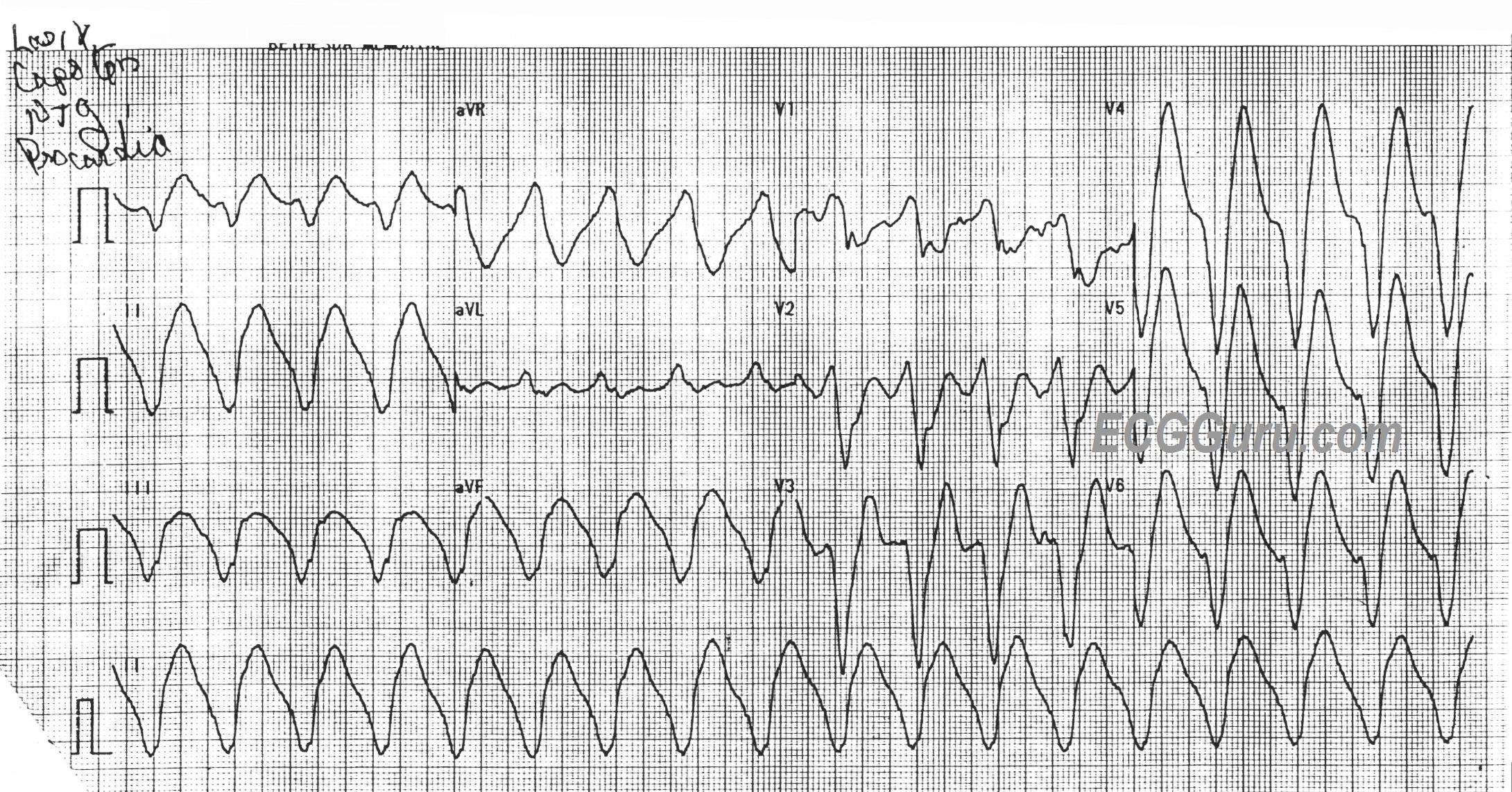
- SUSTAINED VENTRICULAR TACHYCARDIA
- SICK SINUS SYNDROME
- Atrial Flutter With Right Bundle Branch Block and Left Anterior Fascicular Block In a Patient With Preexisting RBBB + LAFB
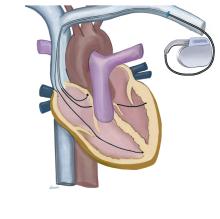
- Ventricular Tachycardia. Unsuccessful Antitachycardia Pacing in an ICD Patient
- High-grade AV Block
- Atrial Flutter Degenerates Into Atrial Fibrillation
- Sinus Bradycardia and More
- SMART WATCH ECG
- Atypical Atrial Flutter (From the Left Atrium)
- Ventricular Tachycardia
- Right Bundle Branch Block